Visualizing the Effect of
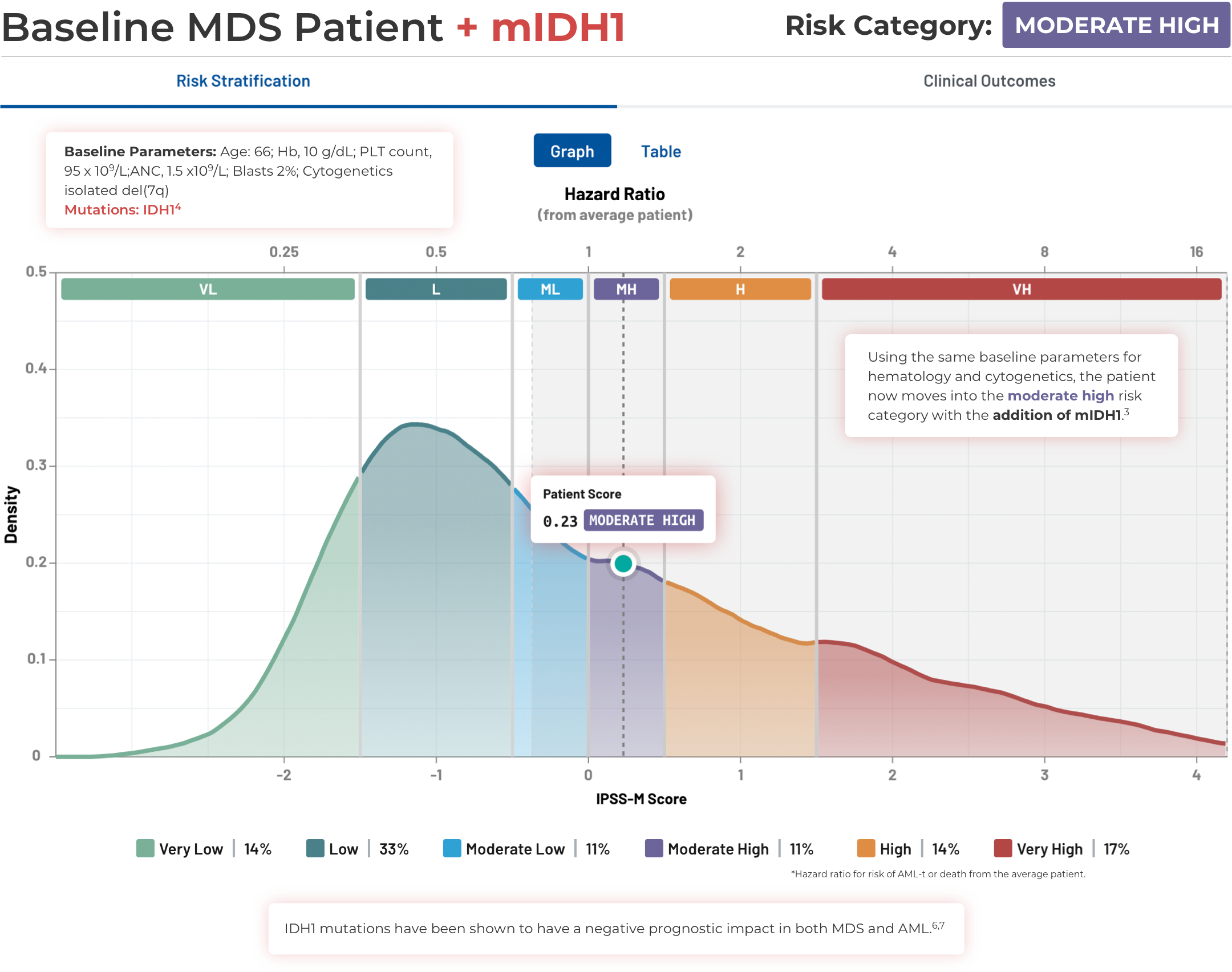
IDH Mutations in MDS
Visualizing the Effect of IDH Mutations in MDS
Using the IPSS-M Risk Calculator
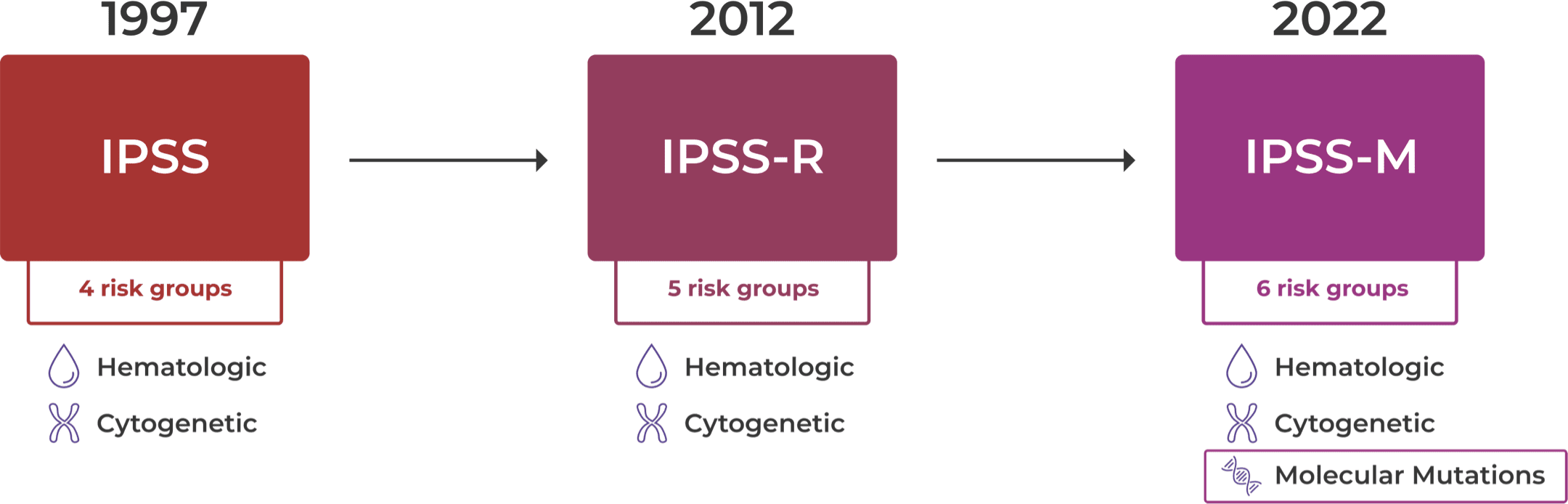
Evolution of the International
Prognostic Scoring System (IPSS)
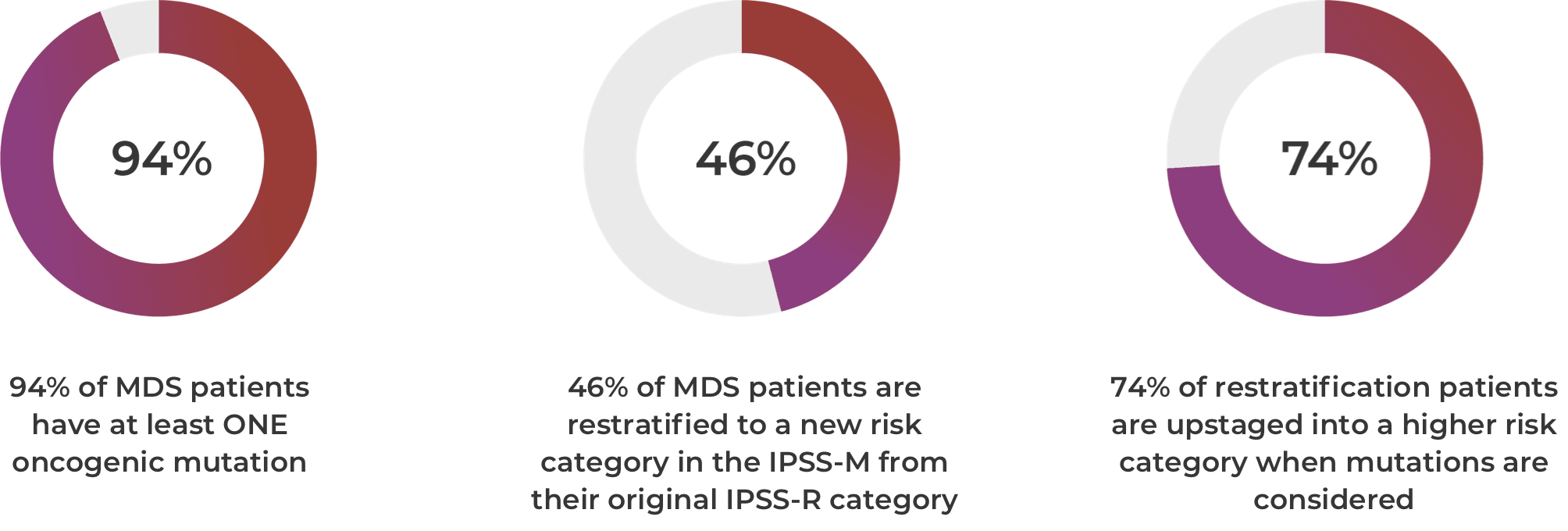
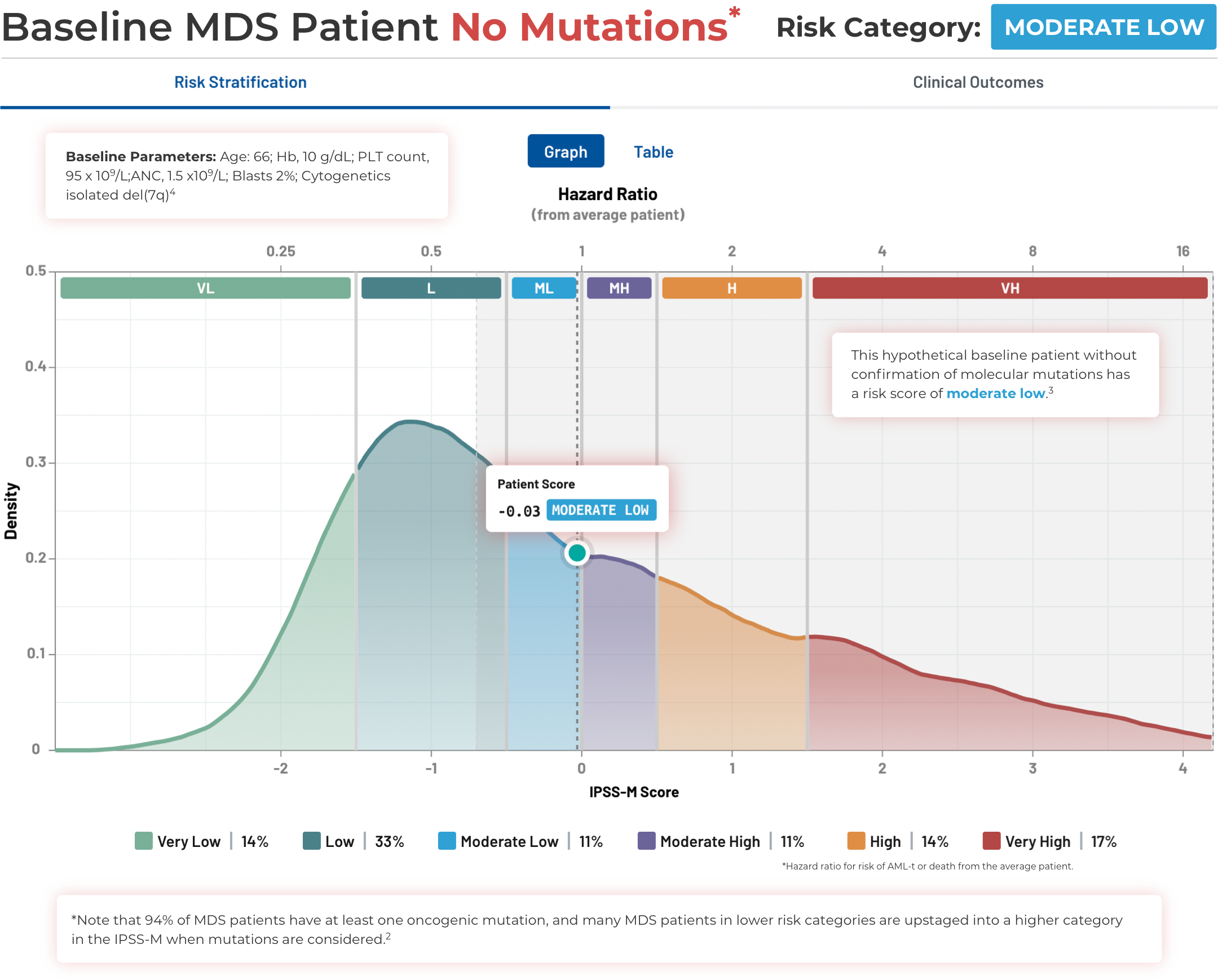
94% of patients with MDS have at least one oncogenic mutation. 46% of patients are restratified to a new risk category in the IPSS-M from their original IPSS-R category. 74% of restratified patients are upstaged into a higher risk category when mutations are considered.2
Key Points
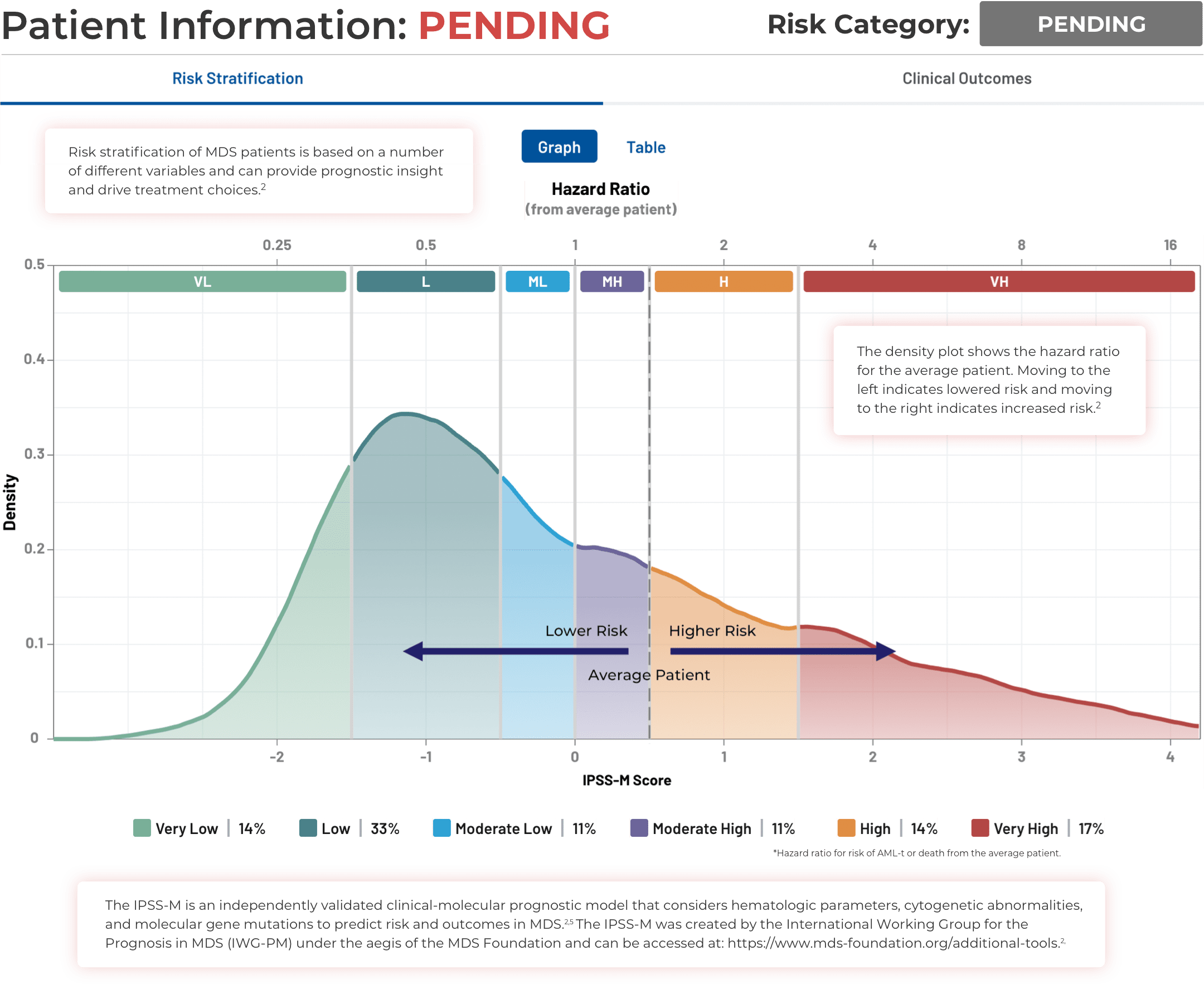
IPSS-M Risk Categories and
Associated Clinical Outcomes2
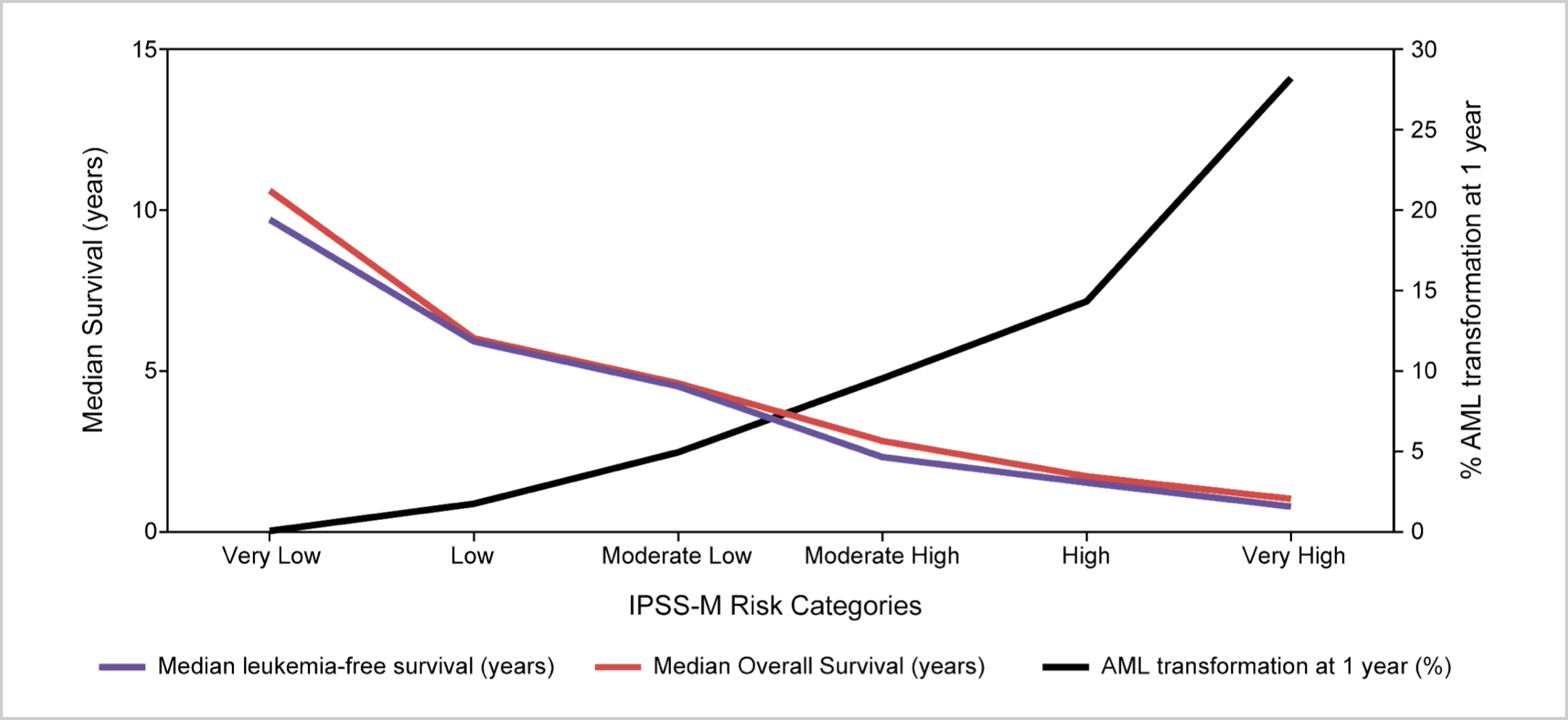
Increased risk category decreases median leukemia-free survival (LFS) and median overall survival (OS) and increases the risk of AML transformation.2
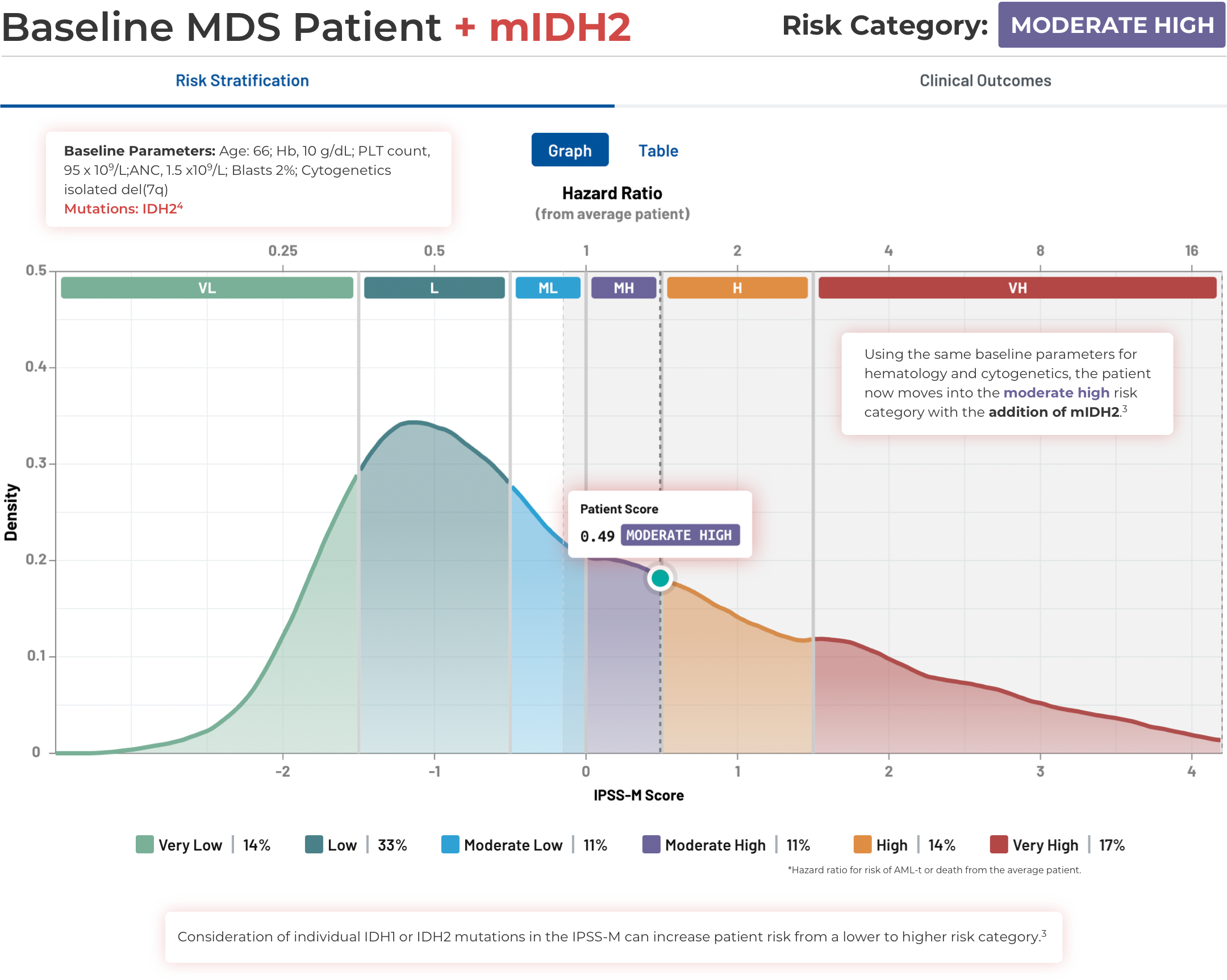
Visualizing the Effect of
Mutations on MDS Patient Risk
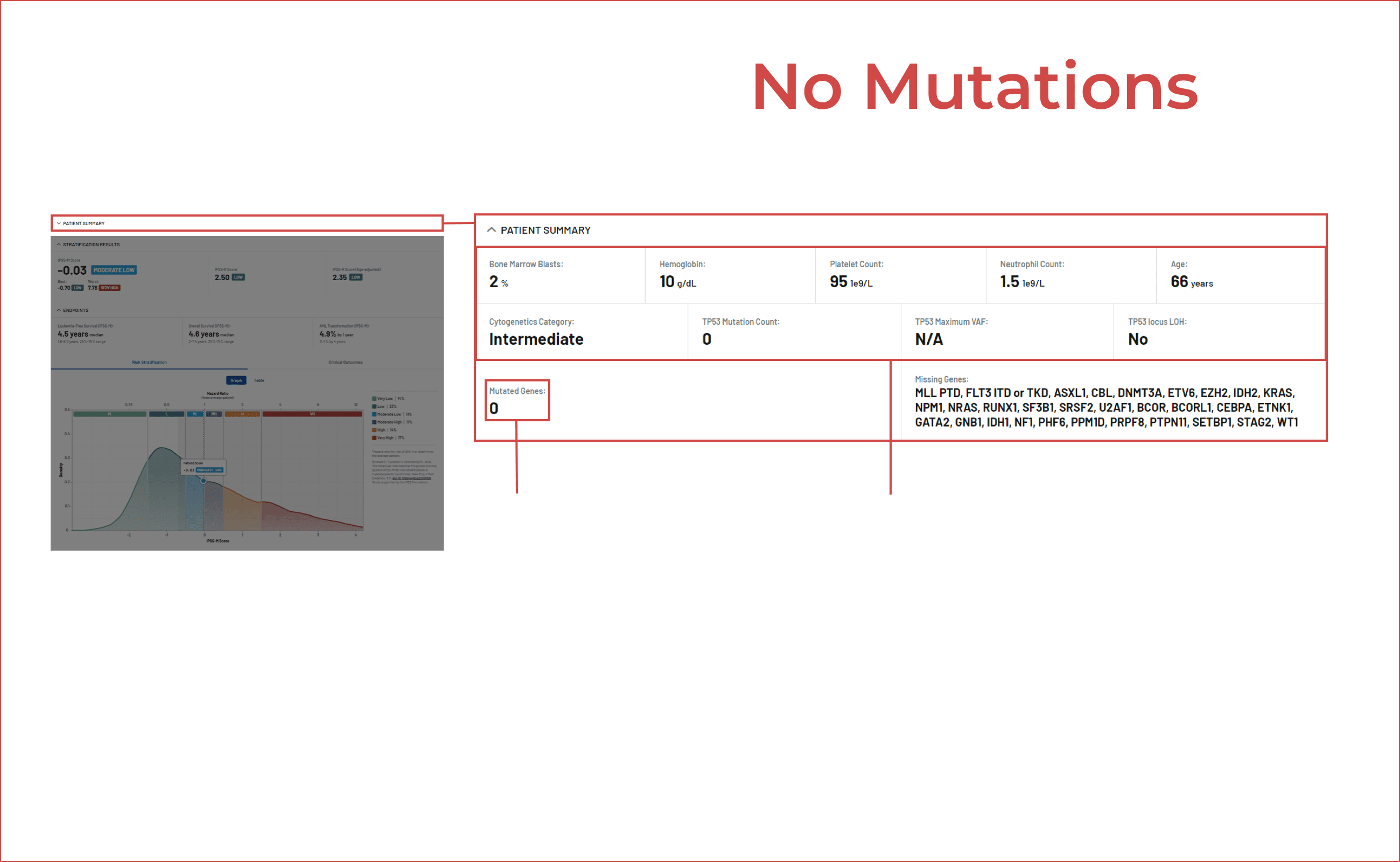
Visualizing the Effect of Mutations on MDS Patient Risk
Using the IPSS-M Risk Calculator
Note that IPSS-M results are less confident with missing mutation data.3
Stay in the Know
Keep up to date on the latest in
IDH science from leading experts.
References:
1. Greenberg PL, Tuechler H, Schanz J, et al. Blood. 2012;120(12):2454-2465. doi:10.1182/blood-2012-03-420489 2. Bernard E, Tuechler H, Greenberg PL, et al. NEJM Evidence. 2022;1(7). doi:10.1056/EVIDoa2200008 3. IPSS-M Risk Calculator website. https://mds-risk-model.com/. Accessed March 25, 2023. 4. Cazzola M. Hematology. 2022;2022(1):375-381. doi:10.1182/hematology.2022000349 5. Aguirre LE, Al Ali N, Sallman DA, et al. Leukemia. Published online May 5, 2023. doi:10.1038/s41375-023-01910-3 6. Thol F, Weissinger EM, Krauter J, et al. Haematologica. 2010;95(10):1668-1674. doi:10.3324/haematol.2010.025494 7. Abbas S, Lugthart S, Kavelaars FG, et al. Blood. 2010;116(12):2122-2126. doi:10.1182/blood-2009-11-250878